Baby’s blue lips can indicate reduced oxygen levels; it’s crucial to seek medical advice.
Understanding Cyanosis in Infants
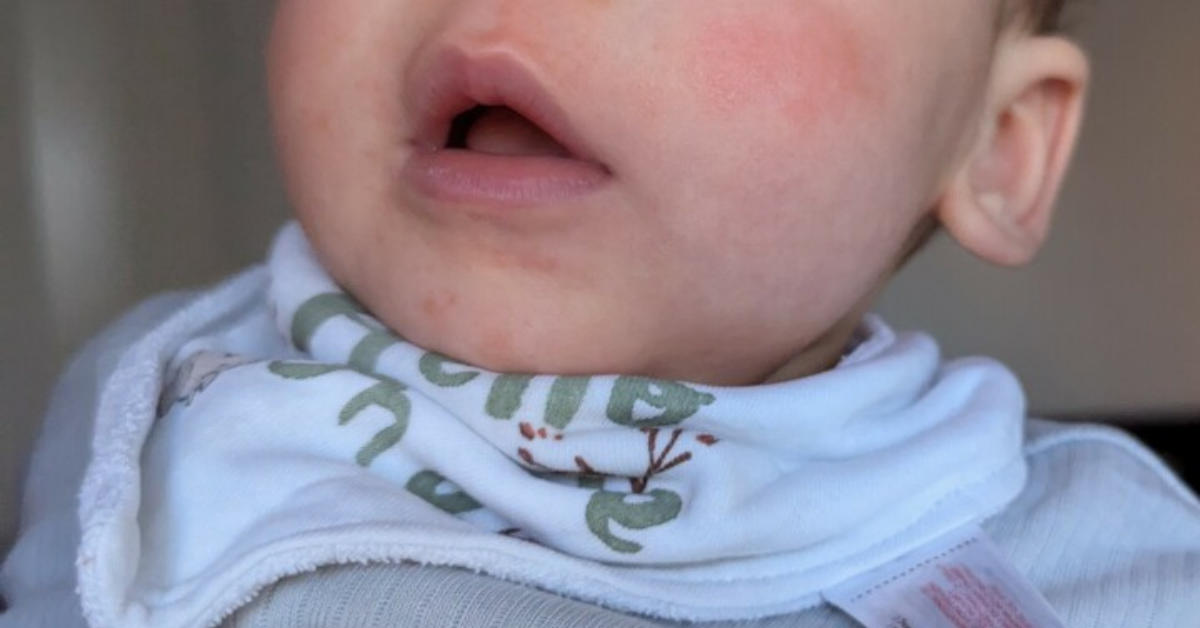
Seeing a baby’s lips turn blue can be alarming for any parent. This phenomenon, known as cyanosis, occurs when there’s inadequate oxygen in the blood. It’s not uncommon for new parents to feel a surge of panic upon witnessing this change in their baby’s appearance. The blue tint can manifest as a result of various conditions, some benign and others more serious. Understanding why this happens is crucial for parents to navigate their child’s health effectively.
| Indicator (at rest) | Possible meaning | Parent action |
|---|---|---|
| Pre-ductal SpO₂ ≥ 95 % | Normal oxygenation. | Routine care. |
| SpO₂ 90–94 % — or blue only after crying/cold, fades quickly | Mild, transient desaturation or acrocyanosis. | Re-check in 5 min; warm baby. |
| SpO₂ 85–89 % or blue tongue/lips at rest | Moderate hypoxemia, possible central cyanosis. | Call pediatrician the same day. |
| SpO₂ < 85 % or blue spell + limp or hard-to-rouse | Severe hypoxemia (tet spell, sepsis, CHD). | Activate emergency services. |
Cyanosis can appear in several forms, primarily central and peripheral cyanosis. Central cyanosis involves the lips and tongue turning blue, indicating systemic oxygen deprivation. Peripheral cyanosis, on the other hand, affects the extremities like fingers and toes. While both types can cause concern, central cyanosis often requires immediate attention. In infants, understanding the underlying causes is essential to address any health issues promptly.
The reasons behind a baby’s blue lips can vary widely. It could be something as simple as exposure to cold temperatures or an indication of a more serious condition like congenital heart defects or respiratory issues. Parents often find themselves worrying about the worst-case scenarios when they see this change in color. Being informed about potential causes helps alleviate some fears and prepares families for necessary medical interventions.
Common Causes of Blue Lips
Several factors contribute to why a baby’s lips might appear blue. One common cause is hypothermia. Babies are especially sensitive to temperature changes due to their small size and limited ability to regulate body heat. If a baby gets too cold, blood vessels constrict, leading to reduced blood flow and oxygen delivery to the skin’s surface—hence the bluish hue.
Another potential cause is respiratory distress. If a baby is fighting to breathe—because of pneumonia, bronchiolitis, or, less commonly in the first year, asthma-like bronchospasm—their body may not get enough oxygen. This lack of oxygen can lead to central cyanosis, where the lips and tongue appear bluish. In such cases, it’s vital for parents to monitor other symptoms like wheezing or rapid breathing.
Congenital heart defects are another serious reason behind blue lips in infants. These defects affect how blood flows through the heart and body, potentially leading to inadequate oxygenation of the blood. Symptoms may include difficulty feeding, excessive sweating during feeds, or lethargy alongside cyanosis. Early detection and intervention are crucial for managing these conditions effectively.
Infections can also play a role in causing cyanosis in babies. Severe infections may lead to sepsis—a life-threatening condition that occurs when the body’s response to infection causes widespread inflammation and organ dysfunction. In such cases, parents might notice other signs like fever or irritability along with blue lips.
Recognising Benign Circumoral Cyanosis vs. Central Red-Flags
Not every dash of blue demands an ambulance. Circumoral cyanosis—a faint bluish ring just outside the vermilion border—often crops up when a baby is cold, crying, or even after a hearty feed, and it fades fast once circulation normalises. The key test is the mucous membrane: if the tongue stays pink, oxygen saturation is usually fine. By contrast, a blue or purple tongue or inner lip signals true central cyanosis and must be treated as an emergency.
The Role of Temperature
Temperature plays a significant role in why a baby’s lips might turn blue. Babies are particularly vulnerable to cold environments due to their limited subcutaneous fat and smaller body mass compared to adults. When exposed to chilly air or water, their bodies prioritize keeping vital organs warm over extremities—this includes the lips.
When babies get cold, peripheral blood vessels constrict as part of the body’s natural response known as vasoconstriction. This process reduces blood flow near the skin’s surface, resulting in a bluish tint on areas like the lips or fingertips while preserving warmth for essential organs such as the heart and brain.
Parents should always be mindful of their baby’s environment during colder months or when transitioning from warm indoor spaces to chilly outdoor conditions. Dressing babies appropriately for weather changes helps prevent unnecessary exposure that could lead them into hypothermic states where lip discoloration might occur.
Keeping an eye on how long a baby spends outside in cooler temperatures can also help prevent these situations from escalating into something more serious—especially if they show signs of discomfort or distress while outdoors.
Signs That Require Immediate Attention
While some instances of blue lips may resolve quickly with warming or repositioning the baby comfortably, certain signs warrant immediate medical attention. If a parent notices that their baby’s lips are persistently blue despite warming efforts or if they exhibit additional symptoms like difficulty breathing or lethargy, seeking help becomes critical.
Other concerning symptoms include excessive fussiness that seems unusual for the child’s typical behavior patterns or if they become unusually sleepy and hard to wake up—these could indicate underlying health issues requiring prompt evaluation by healthcare professionals.
Parents should also pay attention if feeding becomes difficult for their baby either directly (difficulty sucking) or indirectly (fatigue). These signs signal potential respiratory distress that needs further investigation by pediatricians who specialize in infant care.
In instances where bluish discoloration accompanies other significant health concerns—such as rapid heart rate combined with decreased responsiveness—the urgency increases substantially; calling emergency services might be necessary depending on severity levels observed at home before transport occurs.
What Doctors Do: From Pulse-Ox to Echocardiogram
Once you reach the clinic or emergency department, staff run through a rapid protocol:
- Pre- and post-ductal pulse-oximetry. A probe on the right hand and one foot can unmask “differential cyanosis,” a clue to duct-dependent heart lesions.
- Blood gas & hemoglobin panel. These tests confirm hypoxemia and screen for methemoglobinemia or polycythemia.
- Chest X-ray and lung ultrasound. Quick ways to spot pneumonia, effusions, or diaphragmatic hernia.
- Bedside echocardiogram. Shows ductus-dependent flow, Tetralogy of Fallot, or transposition in minutes.
Knowing the steps ahead of time helps parents stay calm and provide a concise history—when did the colour change, did it resolve with crying, what was the baby doing? That history, plus targeted imaging, lets the team separate benign acrocyanosis from life-threatening heart disease in a single visit.
When To Consult A Pediatrician
Consulting a pediatrician is essential whenever there are concerns about why my baby’s lips are blue—especially if it happens frequently without clear explanations like temperature changes! Parents should maintain open lines of communication with healthcare providers regarding any observations related specifically around colour changes experienced by their infants’ skin tone over time frames noted throughout growth milestones achieved during infancy stages.
Regular check-ups allow doctors not only to assess overall development but also to provide guidance on what constitutes normal variations versus concerning symptoms warranting follow-up appointments tailored specifically towards individual needs based upon family histories taken into account during evaluations performed regularly throughout childhood years ahead!
It’s advisable always to err on the side of caution when dealing with young children whose bodies undergo rapid changes constantly—they often don’t exhibit typical signs adults may recognize easily! Keeping track of daily habits surrounding eating patterns and sleeping routines plays vital roles in understanding each child’s unique development journey unfolding before us daily!
Parents should maintain records documenting any instances where discoloration occurs alongside other symptoms witnessed at home before appointments take place so physicians have thorough insights available during consultations scheduled accordingly based upon urgency levels displayed through observations made firsthand prior to visits occurring regularly over time spans covered!
Prevention Strategies for Parents
Smart Monitoring at Home—Without Over-reliance
Direct-to-consumer pulse-ox socks and smart cams can be reassuring, but neither they nor any wearable are recognised as a defence against SIDS or sudden cyanotic spells. False alarms trigger anxiety; missed events breed false security. If families choose a monitor, treat readings below 90 % or trends that dip repeatedly below baseline as a prompt to look at the baby first, not the phone. Normal colour, easy breathing, and good tone outweigh any single number.
Preventing episodes where my baby’s lips turn blue involves taking proactive measures aimed at ensuring optimal health practices within households established early on! Parents must prioritize creating safe environments conducive to promoting well-being across various aspects ranging from nutrition offered throughout infancy stages through appropriate clothing choices made depending on seasonal changes observed locally!
Maintaining stable room temperatures promotes comfort levels necessary for keeping infants relaxed while minimizing risks associated with sudden drops experienced unexpectedly due to environmental factors! Investing in quality clothing designed specifically to protect against cold drafts helps ensure little ones remain cozy regardless of external weather conditions encountered outdoors!
Regularly monitoring feeding schedules ensures babies receive adequate nutrition needed to support growth milestones reached successfully without compromising overall energy levels required to sustain healthy lifestyles maintained throughout early developmental phases! Consulting healthcare providers regarding specific dietary recommendations tailored to individualized needs assists families in making informed decisions based upon unique circumstances faced daily!
Gentle tummy-time, supervised floor play and age-appropriate movement are still great for development, but they are not a substitute for medical evaluation if cyanosis appears.
Key Takeaways: Cyanosis
➤ Blue Lips Indicate Oxygen Issues: Baby’s blue lips may signal low oxygen levels.
➤ Types of Cyanosis: Central cyanosis affects lips; peripheral affects extremities.
➤ Common Causes: Cold exposure, respiratory issues, or congenital heart defects.
➤ Seek Immediate Help: Persistent blue lips with other symptoms need urgent care.
➤ Monitor Environment: Keep temperature and clothing appropriate to avoid cold-induced acrocyanosis.
Frequently Asked Questions: Why Is My Baby’s Lips Blue?
What does it mean when my baby’s lips are blue?
When a baby’s lips turn blue, it indicates cyanosis, which means there is reduced oxygen in the blood. This condition can arise from various factors, including respiratory issues or congenital heart defects. It’s important to monitor other symptoms and consult a healthcare professional if the discoloration persists.
How can I differentiate between central and peripheral cyanosis?
Central cyanosis affects the lips and tongue, indicating systemic oxygen deprivation. In contrast, peripheral cyanosis impacts extremities like fingers and toes. Observing the areas affected can help determine the type of cyanosis and its potential seriousness, guiding parents on when to seek medical attention.
What should I do if my baby’s lips remain blue after warming them?
If your baby’s lips stay blue despite warming efforts, it’s crucial to seek immediate medical help. Persistent cyanosis could signal serious underlying issues such as respiratory distress or congenital heart defects that require prompt evaluation and intervention by healthcare professionals.
Are there specific signs of respiratory distress I should watch for?
Yes, signs of respiratory distress include wheezing, rapid breathing, or difficulty feeding. If your baby exhibits these symptoms alongside blue lips, it’s essential to contact a pediatrician immediately for further assessment to ensure they receive appropriate care without delay.
How can I prevent my baby’s lips from turning blue in cold weather?
To prevent blue lips due to cold exposure, dress your baby warmly in layers suitable for the weather. Keep their environment at a stable temperature and limit time spent outdoors in chilly conditions. Regularly check for signs of discomfort to ensure their well-being during colder months.
Conclusion: Addressing Concerns About Cyanosis
The question “Why Is My Baby’s Lips Blue?” is one that many parents grapple with at some point during early childhood experiences shared together! Understanding potential causes behind these occurrences equips families to better manage situations arising unexpectedly while fostering peace of mind knowing they’re equipped to handle challenges presented along journeys taken towards nurturing healthy, happy children growing up strong, resilient individuals capable of thriving in the future ahead!
Being informed about warning signs and seeking help promptly ensures timely interventions occur whenever necessary, safeguarding precious lives entrusted to our care, ultimately leading to brighter tomorrows filled with laughter and joy, cherished memories created in moments spent together exploring the world around us every day anew!